
1Įmergency departments are overused in multiple ways-varying levels of severity including acute conditions, acute on chronic illnesses, mental health, substance abuse, and prescription refills, among others. Volatility and continuously rising costs in the United States healthcare system have created a marketplace in which urgent care centers can play an essential role by helping to reduce cost, increase patient satisfaction, and improve outcomes.Īt the same time, overwhelmed emergency departments need help in minimizing low-acuity/unnecessary usage while reducing cost and assisting in health disparities.Īccording to the Centers for Medicare and Medicaid Services (CMS), healthcare spending is expected to increase to 19.4% from 17.9% in the next 7 years, giving UCCs the opportunity to step up in cost-reducing actions.

Reducing low-acuity preventable emergency room visits by utilizing urgent care center services via mobile health unit diversion program. The creation of a mobile health diversion program to transport low acuity conditions to urgent care instead of a hospital emergency department can improve population health and reduce healthcare cost providing the opportunity to leverage value-based care by targeting the triple aim (reducing cost, increasing patient satisfaction, and improving outcomes) while freeing up the emergency medical system services.Ĭitation: Jaramillo CM. An assessment of peak activity reveals that Virginia saw a spike in preventable ED diagnoses in March 2016, followed by a downward trend in the summer months, then an uptick during the winter.Urgent message: Urgent care centers can execute and implement innovative ideas to ameliorate overcrowded Emergency Rooms. Evaluating the data on a regional basis, the Eastern region (most populous) and the Southwestern region (least populous) are the top areas of the state for preventable ED visits, accounting for 47 percent of all such visits identified in the state. Those conditions account for 66 percent of the top 10 conditions linked to preventable ED visits in Virginia. Key findings from the analysis of 2016 data demonstrate that diagnoses for sprains, urinary tract infections, and acute bronchitis were the top three conditions associated with preventable ED visits. 3 To examine preventable ED visits in Virginia, the VHHA Analytics Team leveraged the All-Payer Claims Database (APCD) – it contains 99 percent of Medicare and Medicaid claims and roughly 50 percent of commercial claims – to conduct an analysis of trends in the Commonwealth. 2 It is estimated that as many as 20 percent of ED visits for non-emergency conditions could be resolved in a retail clinic or urgent care center, an outcome that could generate as much as $4.4 billion in annual cost savings.

For instance, a 2012 BMC Health Services Research study identified three consistent themes linked to ED misuse: patient belief that visits will satisfy an immediate need such as pain alleviation the presence of barriers to care access from primary care providers or other outpatient treatment patient perception that an ED visit is convenient.
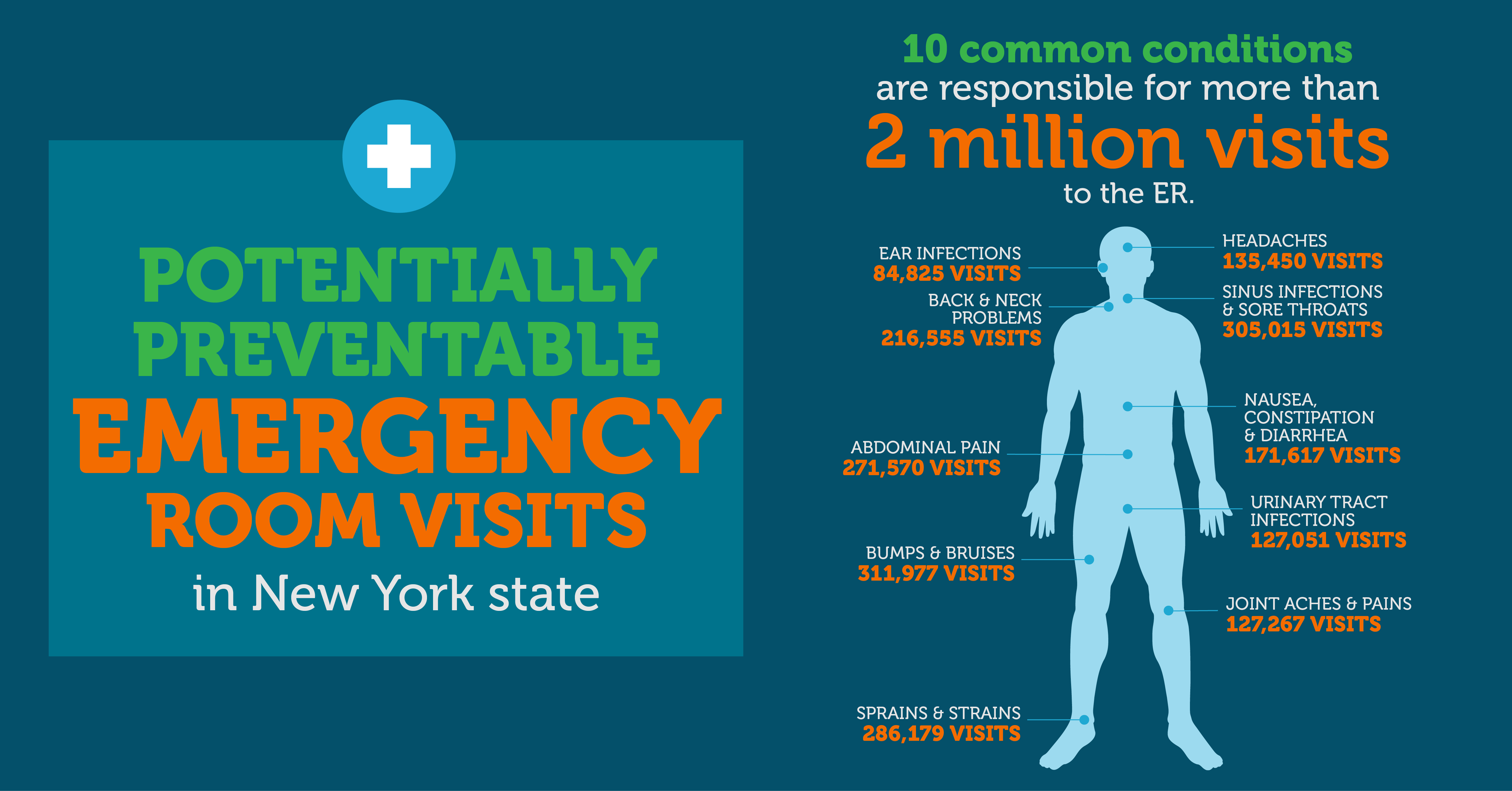
1 Many factors contribute to patients seeking ED care for non-emergencies. A preventable emergency department (ED) visit occurs when a patient seeks ED treatment for a health condition that can be treated in a non-emergency setting or avoided due to previous preventive care.


 0 kommentar(er)
0 kommentar(er)
